 (CNN) —
(CNN) — The latest “it” ingredient to hit menus is CBD, short for cannabidiol,
one of over 60 cannabinoids found in the cannabis sativa plant (more commonly known as marijuana).
Unlike THC, the most well-known cannabinoid, CBD has no psychoactive effects. So, while it won’t get you high, its reported therapeutic properties have driven CBD sales and popularity in the wellness industry.
While researchers are still trying to determine CBD’s effects, some studies suggest it can help treat inflammation, pain, anxiety and seizures.
The controversy around this superfood stems from inconsistent cannabis regulation at the federal and state level. Despite growing legalization, the DEA still considers cannabis — including CBD, unless sourced from industrial hemp —
an illegal drug.
To date, the FDA hasn’t approved any CBD products apart from an epilepsy drug called
Epidiolex. State laws vary and are changing all the time.
Take California, a state with legalized recreational cannabis and a famously vibrant cannabis cuisine scene: Just this summer, the California Department of Public Health stopped the sale of CBD additives in
food and drink until it receives full FDA approval.
This left restaurants such as Gracias Madre and Superba Food + Bread scrambling to change their menus to accommodate the rule.
With the Golden State out of the culinary cannabis spotlight at the moment, it’s time to highlight some other less celebrated locations where you can find CBD-infused treats out in the wild.
From a sleek, wellness compound in Miami to a Portland dive bar known for late-night hot dogs, here are the coolest spots to find CBD on the menu (for now).
Adriaen Block, Queens, NY
Adriaen Block’s CBD Negroni.
Lily Brown/Adriaen Block
This newly opened Queens cocktail bar and restaurant is a CBD mecca, showcasing the ingredient front and center.
For the uninitiated, the menu offers a word of advice: “CBD will not get you high, but you may experience a calming sensation.”
The infused drinks include the Stoney Negroni, Rolled Fashioned, and the Bakin’ & Eggs, which is made with Pineau des Charente, Lillet Blanc, blood orange bitters, egg white, and garnished with crisped bacon.
Teetotalers can get in on the action too, thanks to an equally thoughtful selection of CBD mocktails made with Seedlip, a swanky, non-alcoholic distilled spirit. Not thirsty? Also on offer are entrees with a side of AB CBD sauce or a pillowy blob of CBD-infused whipped cream to top off dessert.
Adriaen Block, 19-33 Ditmars Blvd, Astoria, NY 11105, +1 (718) 686-1391
Broomwagon, Lexington, KY
A community mecca for bike culture, this bicycle shop is also a beer garden and café serving up locally-sourced coffee, creative comfort food and ice-cold crafts and drafts.
Customers bringing in their bike for repairs can enjoy a snack by the mechanic’s work area while they wait, or check out the latest wheels and accessories. (New pannier bag, anyone?)
They’ll add a dose of CBD to any beverage for $2, or you can order a specialty drink like the Sage Advice Latte, with maple and sage-infused syrup, espresso, steamed milk and CBD.
Koku, Brooklyn, NY
This Kokus Zen bowl delivers on its name.
Courtesy Kokus
Think of the Zen Bowl as an ice cream sundae for the Goop set — dairy-free, probiotic-enriched coconut soft-serve heaped with colorful superfood toppings like antioxidant blueberries, nutritious black sesame granola and CBD cacao magic shell.
Available April through October at Brooklyn’s Smorgasburg on Saturdays in Williamsburg and Sundays in Prospect Park, it’s allergy-free and utterly Instagrammable.
You can also find the frozen treat at sporadic pop-ups (check their website for upcoming events), but stay tuned: A brick and mortar location is in the works for next year.
Donnie Vegas, Portland, OR
The coolest downtown Las Vegas dive bar is actually located in Northeast Portland, serving cocktails on tap and cheap, creative hot dogs like the Seoul Dog (kimchi, sambal aioli, scallion) and Tijuana Dog (cream cheese, pico de gallo, jalepeno) until 2:30 am.
They offer Jell-O shots and wine in a can, and a slushee with a hemp-derived twist — the Prickly Pear CBD Margaweeda, made with fresh lime juice, triple sec, silver tequila and prickly pear puree.
Donnie Vegas, 1203 NE Alberta St, Portland, OR 97211, +1 (503) 477-7244
Green Goddess Cafe, Stowe, VT
This homey café, a neighborhood go-to for fresh-pressed juices and tasty breakfast scrambles, was one the first in Vermont to put the wellness ingredient on the menu after “we experienced the benefits of CBD firsthand with our son, who has autism and a tumor disorder,” owner Athena Scheidet says.
One of their most popular specialty drinks is the Jamaican Me Shake, a CBD smoothie with tropical fruit, spinach, avocado, organic apple juice and whipped cream.
The James New York NoMad, New York City
The James NoMad brings CBD to R-n-R.
Courtesy The James Nomad
Travelers who want a break from Manhattan’s hectic pace don’t even need to leave their boutique hotel room for the latest way to unwind — CBD-infused room service from notable cannabis chef Annabel Drummer.
The in-room dining menu includes spicy meatballs, gorgonzola salad with walnuts and pear, and house tater tots. Or, you can pick a prepackaged CBD-infused treat like Chef For Higher Gummies, Grön Chocolate bars, and even Bark Avenue dog treats for stressed pets.
VegeNation, Las Vegas
Stay hydrated in Vegas with this whiskey CBD tea.
Courtesy Vege Nation
Downtown Las Vegas’s Fremont East area has become an artsy hub for plant-based eats and health-conscious cocktails — the antithesis of the Strip’s bottle service and Champagne-shower decadence.
Affordable global street food at VegeNation is locally grown and plant-based, and even the cocktails have a positive spin — particularly The Changemaker, a refreshing, infused whiskey tea made with local distilled liquor and tea from Bloomin’ Desert Herb Farm, a brew of rosemary, ginger, holy basil, red clover, nettle, peppermint, clove and raw CBD oil in purified water.
VegeNation, 616 Carson Ave #120, Las Vegas, NV 89101, +1 (702) 366-8515
Plant Miami, Miami
The secret ingredient in Plant Miami’s drink isn’t so secret.
Courtesy Plant Miami
Miami isn’t all neon lights, and pumping basslines. When the South Beach scene feels like it’s all too much, find your Zen at Sacred Space Miami.
The minimalist oasis in once-gritty Wynwood features a lush meditation garden, yoga and wellness classes, and Plant Miami, an organic, vegan farm-to-table restaurant.
The tropical Plant Medicine cocktail — with fresh pineapple, house coconut milk, dark rum, and a dose of CBD oil — is the perfect blend of Miami vibes and mindfulness.
Plant Miami, 105 Northeast 24th St, Miami, FL, 33137, +1 786 621 5006
River and Woods, Boulder
The comfort food at this historic cottage includes community-sourced dishes like Aunt Penny’s Mac & Cheese with mushrooms and onion-potato crunch and John’s Gnocchi Verde with spinach, Reggiano cream, and lemon zest.
There are family-friendly picnic tables in back, as well as an adult-centric Airstream that serves as an outdoor bar, where you can add a dose of CBD to cocktails like the Sloe Descent, with Luxardo amaretto, Spirit Works sloe gin, orange and pomegranate juice.
(They’re in the process of formulating a dedicated CBD-infused wellness cocktail, too.)
Coalition Brewing, Portland, OR
IPA + CBD = Coalition Brewing’s Two Flowers brew.
Courtesy Coalition Brewing
This brewery changed the game with Oregon’s first commercially produced CBD-infused beer, Two Flowers IPA, highlighting the kinship between cannabis and hops with an aromatic, grassy flavor.
The beer has become so popular that you can find it all over town at establishments like EastBurn Public House and Dot’s Café, though it’s worth a visit to the tasting room’s new patio where you can enjoy it in its original birthplace.
Zenbarn, Waterbury, VT 05676
Yes, even your burger can help you chill.
Courtesy ZenBarn
You haven’t reached peak Vermont until you’ve visited this rustic barn-turned-restaurant’s periodic “Hemp and Hops” dinners, where five-course meals are infused with CBD and paired with local craft beers.
It’s a community-focused space, with a yoga studio upstairs and live music at night. (Be prepared to hear Grateful Dead covers.)
The daily menu offers CBD-spiked aioli for their burgers, including the vegetarian Zen Burger, a local black bean patty piled with cheddar, chipotle crema, avocado, lettuce, and crispy onion.
There’s also CBD honey vinaigrette for salad, a CBD brownie sundae with house-made CBD caramel, and clever CBD cocktails with names like Gin and Chronic, Le Verde and Up in Smoke.
Zenbarn, 179 Guptil Rd, Waterbury Center, VT 05677, +1 (802) 244-8134
Grön Cafe Portland, OR
Grön serves its CBD on the sweet side.
Courtesy Gron
If there was a Willy Wonka of cannabidiol, it would Christine Smith, founder of craft chocolate company GrönCBD.
The manufactory’s confections contain CBD extracted from a hemp alternative — evergreen tree bark combined with citrus peels.
The front of house is a drop-in cafe, where you can order CBD Drinking Chocolate served with whipped cream and a shortbread cookie, as well as infused chocolate lattes, steamers, iced chocolate drinks, chocolate-filled croissants, and truffles.
They’ll indulge your curiosity and your sweet tooth — visitors are encouraged to ask questions or sample the CBD caramel and chocolate sauces, chocolate bars, tinctures and body products.
 (CNN) — The latest “it” ingredient to hit menus is CBD, short for cannabidiol, one of over 60 cannabinoids found in the cannabis sativa plant (more commonly known as marijuana).
(CNN) — The latest “it” ingredient to hit menus is CBD, short for cannabidiol, one of over 60 cannabinoids found in the cannabis sativa plant (more commonly known as marijuana).










 The first prescription medication extracted from the marijuana plant is poised to land on pharmacists’ shelves this fall. Epidiolex, made from purified cannabidiol, or CBD, a compound found in the cannabis plant,
The first prescription medication extracted from the marijuana plant is poised to land on pharmacists’ shelves this fall. Epidiolex, made from purified cannabidiol, or CBD, a compound found in the cannabis plant,



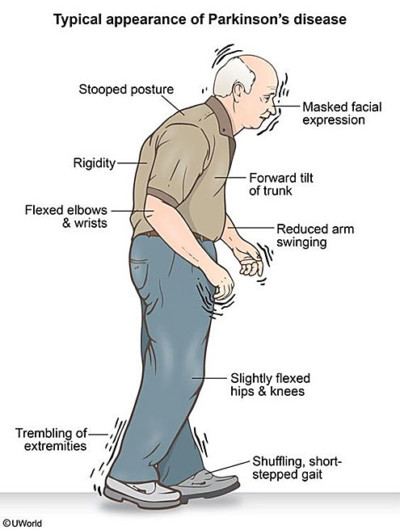
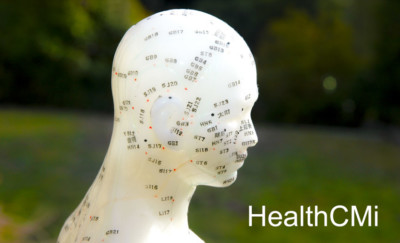 Acupuncture is an effective treatment modality for the alleviation of Parkinson’s disease. Zhejiang University of Traditional Chinese Medicine (Hangzhou, China) researchers conducted a study comparing the effects of drug therapy as a standalone procedure with acupuncture plus drug therapy in an integrated treatment protocol. Based on the data, the researchers conclude that acupuncture plus antiparkinsonian drug therapy is significantly more effective than using only antiparkinsonian drug therapy. [1]
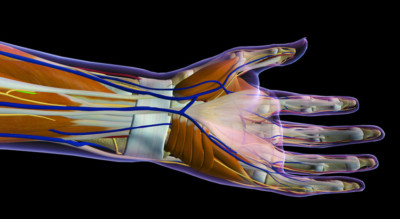
Acupuncture is an effective treatment modality for the alleviation of Parkinson’s disease. Zhejiang University of Traditional Chinese Medicine (Hangzhou, China) researchers conducted a study comparing the effects of drug therapy as a standalone procedure with acupuncture plus drug therapy in an integrated treatment protocol. Based on the data, the researchers conclude that acupuncture plus antiparkinsonian drug therapy is significantly more effective than using only antiparkinsonian drug therapy. [1] Traditional Chinese medical treatments have been around for millennia – and embraced the world over.Scientists, however, are skeptics by profession and look for that ultimate seal of approval: “proof.”As CGTN’s Frances Kuo reports, researchers are stepping up to the challenge and finding some success linking traditional methods to modern science.Acupuncture originated in China thousands of years ago and is popular today all over the world.Practitioners insert thin needles through the skin of a patient, stimulating what they call “acupoints” – to improve a whole host of conditions.But despite generations of anecdotal accounts of its effectiveness, there’s never been absolute scientific proof that it works.Recently though, Chinese scientists have made breakthroughs in understanding.Key to acupuncture’s effectiveness is the location of the acupoints, found where there are concentrations of human mast cells tied to our immune system.“The Mast Cell has a kind of sensitive protein that can feel the stimulation,” said Huang Meng, Research Assistant at Fudan University. “When it’s activated, the cell releases a kind of bio-active matter, which will, in turn, stimulate the blood capillaries and nerves around it. This will produce a signal for the curative effect.”
Traditional Chinese medical treatments have been around for millennia – and embraced the world over.Scientists, however, are skeptics by profession and look for that ultimate seal of approval: “proof.”As CGTN’s Frances Kuo reports, researchers are stepping up to the challenge and finding some success linking traditional methods to modern science.Acupuncture originated in China thousands of years ago and is popular today all over the world.Practitioners insert thin needles through the skin of a patient, stimulating what they call “acupoints” – to improve a whole host of conditions.But despite generations of anecdotal accounts of its effectiveness, there’s never been absolute scientific proof that it works.Recently though, Chinese scientists have made breakthroughs in understanding.Key to acupuncture’s effectiveness is the location of the acupoints, found where there are concentrations of human mast cells tied to our immune system.“The Mast Cell has a kind of sensitive protein that can feel the stimulation,” said Huang Meng, Research Assistant at Fudan University. “When it’s activated, the cell releases a kind of bio-active matter, which will, in turn, stimulate the blood capillaries and nerves around it. This will produce a signal for the curative effect.”