 By Gabrielle Kassel November 12, 2019 for Shape Magazine
By Gabrielle Kassel November 12, 2019 for Shape Magazine
From CBD lube and clit vibes to intimacy apps and O-shots, there are all sorts of new products popping up promising to improve your sex life. But there’s an ancient treatment method you’re probably sleeping on that could make an even bigger difference: acupuncture.
If you’re scratching your head thinking, “Really?” keep reading. Below, experts explain what acupuncture is exactly and how it may help make your sex life *Daft Punk voice* wetter, better, faster, stronger.
How Acupuncture Can Improve Sexual Functioning
At its most basic, acupuncture involves placing thin, hair-like needles at specific points in the body. The point “is to prompt the body’s own healing abilities to restore balance,” says Jill Blakeway, D.A.C.M., a doctor of acupuncture and Chinese medicine at the YinOva Center in New York City.
That may sound a little woo-woo but research points to acupuncture as having some serious benefits. To name a few, studies show acupuncture has the potential to help with: allergies, fertility issues, symptoms of PMS, headaches and migraines, insomnia, stress, anxiety and depression, and back pain.
Anecdotally, Blakeway adds that she’s also seen people find relief from autoimmune diseases, hormone imbalances, digestives problems (such as acid reflux or IBS), chronic urinary tract infections, chronic cough, and more.
Okay, so where does sex come into all of this? “There are often multiple factors that contribute to sexual problems—many of which acupuncture addresses,” says Blakeway. An in-depth look below.
1. When Stress Increases, Sex Drive Decreases
This won’t surprise you: Higher stress levels are linked to reduced interest in sex, according to a 2018 study published in Archives of Sexual Behavior. (Shocking, I know.)
What does this have to do with acupuncture? Well, when you’re stressed, your body can literally hold that stress as physical tension in your muscles—especially your shoulders, head, and neck, says Blakeway. “You can use acupuncture to relieve stress and tension in those areas,” she says. And as your stress levels go down, your sex drive goes up.
“If low libido is caused by physical stress, then just three or five acupuncture sessions should be enough to bring it back up,” says Irina Logman, certified acupuncturist and owner of Advanced Holistic Center in NYC. But if you’re chronically stressed it may take ten or even twenty sessions to restore it, she says.
Stress, as you’re well aware, can also manifest psychologically. “When you’re stressed, intrusive thoughts can keep you from being in the moment during sex,” says Blakeway. Acupuncture doesn’t just relieve muscular stress; research shows it can also promote mental clarity and relaxation and decrease psychological stress, she says. (BTW: Exercise, unplugging, and breathing can also help you destress.)
2. Blood Flow Everywhere = Blood Flow to Genitals
During an acupuncture treatment, your body sends blood to where it’s being poked it with needles (called acupoints), which Blakeway says, which can improve overall circulation.
Wondering how that could possibly have a positive impact on sexual response? Well, because blood flow to the genitals is a prerequisite to sexual pleasure. One study published in the journal Fertility and Sterility showed that adequate blood flow is responsible for the lengthening of the vaginal canal (making room for penetration) and producing natural lubrication, both of which are hugely important to your body’s preparation for and enjoying of sex. (That’s one reason exercise makes great foreplay, too.)
Sure, this is why folks with circulation disorders and cardiovascular disease often experience sexual dysfunction, but anyone without these illnesses can experience it, too. (Here’s everything you need to know about sexual dysfunction and what it means, exactly.) “So many people nowadays spend much of their workdays sitting, which can cause reduced blood circulation in the pelvic area,” says Logman. Luckily, she says, if the problem has not turned into a chronic condition, “just a couple acupuncture sessions can fix it right up.”
3. Needles + Hormone Balance
It probably isn’t news to you that your hormones, which affect your stress levels, sleep patterns, metabolism, cycle, and food cravings, also affect your sex drive. Luckily, “acupuncture can be used—usually in combination with Chinese herbs—to resolve hormonal problems that can be at the root of a low sex drive,” according to Blakeway.
And research backs that up: A 2018 study published the journal Evidence-Based Complementary Alternative Medicine found that acupuncture can increase estrogen, estradiol, and progesterone, which have been linked to increased sexual desire in women. While the researchers didn’t go as far as to call acupuncture a cure for sex-hormone imbalances, they do say that acupuncture could be part of a holistic approach to hormone therapy.
4. Acupuncture > Side Effects
Another known cause of low libido is anti-anxiety and anti-depressant medication.
Good news: Acupuncture may actually help remedy sexual disorders (think: impotence, loss of libido, and then the inability to orgasm) caused by certain anti-anxiety/depressant meds, according to a study published in the Journal of Alternative and Complementary Medicine.
For the study, folks answered a questionnaire, underwent 12 weeks of acupuncture, and then re-answered the questionnaire. The researchers wrote that the “female participants reported a significant improvement in libido and lubrication” after the 12 weeks of treatment. Possible this was just the placebo effect? Sure, but if people actually noticed an increased libido and had an easier time cumming, IMHO, who cares if it was from the acupuncture or not.
5. Keep Your Partner ⥣
If you’re sleeping with a person with a penis and your bedroom woes include them blasting off before you’re even warmed up, know this: One 2017 review published in the journal Sexual Medicine concluded that acupuncture may help treat premature ejaculation. So, you might get them a few sessions as a gift or, have them tag along to your appointment.
Should You Try Acupuncture for Better Sex?
If you suspect your sex life is ~blah~ because you’re just not that into your partner, you two could communicate better, or you don’t know what brings you pleasure, acupuncture isn’t your solution. (Though, some solo sessions, a break-up, and/or couples therapy might be.)
But, if you have a sit-all-day lifestyle, would self-identify as a Stress Case, think your hormones could be out of whack, or experienced a change in sexual functioning after starting antidepressants or anti-anxiety medication, there’s really no downside to trying it. There may be a little bit of blood or bruising at the site the needle goes in, and some folks report feeling sleepy after their appointment. (Oh, and acupuncture might make you cry.) But any side effects worse than that are rare, according to the experts.
How Long Does It Take for the Acupuncture Benefit to Work?
“Over the years, I treated patients who felt marked improvement after just one session,” says Logman. But it’s not typically that quick of a fix. Blakeway recommends sticking with it for at least six weeks to see a change.
If after six weeks you don’t notice any improvements, Logman suggests going to a professional who uses acupuncture alongside other staples in Traditional Chinese Medicine (such as acupressure, Gua Sha, and more.)
Or, just saying, you can always try another ancient practice: tantric sex. https://www.lucypostolovacupuncture.com/
By Gabrielle Kassel







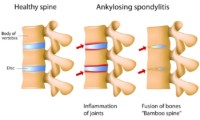 Acupuncture and herbs outperform sulfasalazine for the alleviation of ankylosing spondylitis. Henan University of Traditional Chinese Medicine researchers investigated the benefits of drugs, acupuncture, and herbal medicine for the treatment of ankylosing spondylitis. The researchers conclude that acupuncture plus herbs is more effective than the sulfasalazine (an antirheumatic medication).
Acupuncture and herbs outperform sulfasalazine for the alleviation of ankylosing spondylitis. Henan University of Traditional Chinese Medicine researchers investigated the benefits of drugs, acupuncture, and herbal medicine for the treatment of ankylosing spondylitis. The researchers conclude that acupuncture plus herbs is more effective than the sulfasalazine (an antirheumatic medication).